Author: Trevor Parmer, LD&B Employee Benefits Consultant
The Complex World of Prescription Drugs
Who profits most from the complex world of prescription drug use in an employer-based health plan? The short and unfortunate answer, not the employer and their employees.
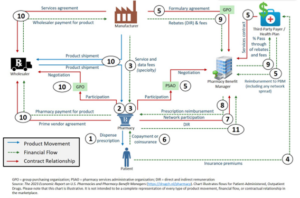
In a typical employer health plan prescription drugs make up 20-25% of the total claims spend and this number continues to increase annually. The complexity of the supply chain (illustration below) leaves room for built-in inefficiencies, which can typically lead to the patient paying the price, with low access and high costs for their medication.
In addition, due to misalignment between key stakeholders in the US pharmaceutical value chain, employers see increased costs and patients are confronted with affordability barriers, leading to prescription abandonment, poor clinical outcomes, and frustrated patients (employees).
Introducing a third-party vendor that is independent of this system for oversight, utilizing transparent pass-through Pharmacy Benefit Managers (PBMs), and technology can hold these stakeholders accountable to ultimately bring greater transparency, savings, and accessibility to your pharmacy benefits.
LD&B’s Employers Health Risk Consortium (EHRC) is a real-life example showing the impact of thoughtful utilization of these tools and the impact they have on a health plan. In the EHRC, we use a pass-through PBM and an independent third party for oversight including special programs, resulting in an average pharmacy spend of 15.0% versus 22.5%* nationally using traditional methods. Reach out to an LD&B Consultant today to learn more!
*Milliman, 2023

 (540) 433-2796 |
(540) 433-2796 |